As of 10 March 2020, over 100,000 people have been infected with the deadly and contagious COVID-19, also known as the novel coronavirus. The severe acute respiratory syndrome (SARS)-like disease is a type of coronavirus that infects humans, bats and other mammals, and has killed over 4,000 people worldwide. Since the virus emerged in Wuhan, China, scientists from different nations have been racing to develop a vaccine to fight the deadly disease. Fortunately, according to Chinese health officials, research on coronavirus vaccines is well under way and will be available for emergency and clinical research use in April.
Developing vaccines that are safe and effective takes time, investment and good science. According to media reports, the testing for a COVID-19 vaccine to ensure its efficacy will take around 12 to 18 months.
Vaccination is one of the most effective ways to prevent disease as it helps the body’s immune system to recognise and fight pathogens like viruses and bacteria, says the World Health Organisation (WHO). In recent years, many vaccines have been developed to protect humans – especially children – from life-threatening diseases such as measles, polio, influenza and cervical cancer.
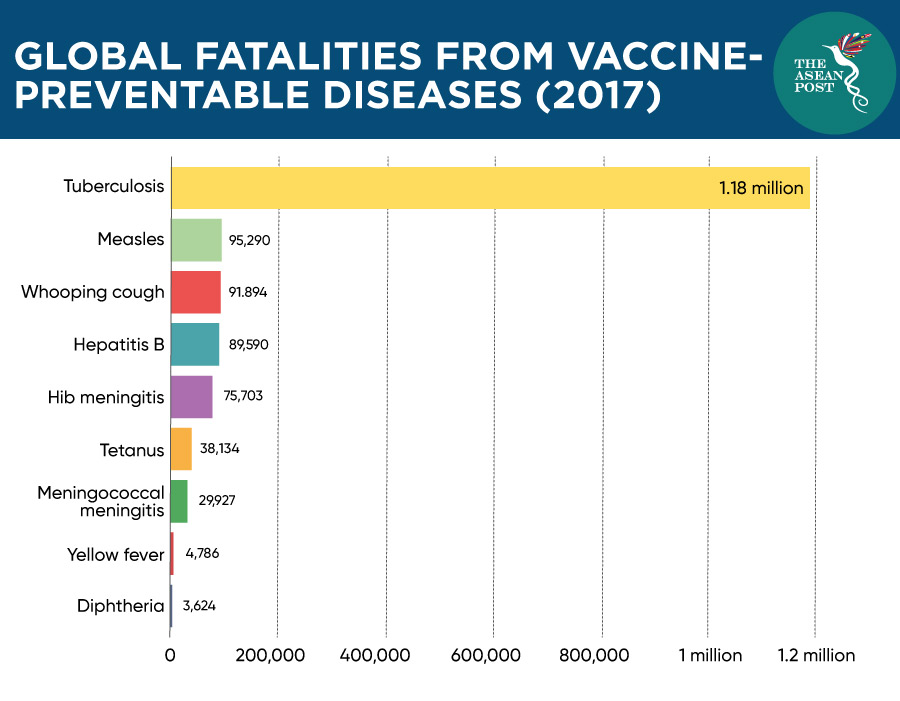
The WHO estimates that at least 10 million deaths were prevented between 2010 and 2015 because of vaccines, with millions more lives protected from vaccine-preventable diseases (VPD). Nevertheless, many people have yet to receive the immunisation vaccines that are available to them.
In 2018, around 19.4 million infants across the globe did not receive routine immunisation services such as the three doses of the DTP (diphtheria, tetanus toxoids and pertussis) vaccine. Around 60 percent of these children live in 10 countries including ASEAN member states Indonesia, the Philippines and Vietnam. The WHO has listed vaccine hesitancy as one of the top 10 threats to global health in 2019.
Vaccine hesitancy
Dengue is not an uncommon disease in the Philippines as thousands of people have been infected with it throughout the years. Last year, the Philippines Department of Health even declared a national dengue epidemic after 414,532 people were infected with the virus and over 1,000 deaths were recorded by November 2019.
So, when French pharmaceutical company Sanofi introduced its dengue vaccine, Dengvaxia in 2016, the Philippines Department of Health was reported to have spent US$67 million on the vaccine. The country then kicked-off a mass immunisation programme with the aim of vaccinating a million students by the end of 2016. A few months later, more than 800,000 children had received at least one of the doses of the vaccine.
However, the Philippines then suspended the sale and distribution of the vaccine after the drug maker warned it could worsen symptoms for people who had not been previously infected. This alarmed parents whose children had been vaccinated. Some politicians and the local media there even linked several deaths to the vaccine. This developed a distrust of vaccines in the nation and fuelled anti-vaccine fears which led to a rise in the number of measles cases in the Philippines.
“The number of cases of measles and other vaccine-preventable diseases has been going up while vaccination rates are going down,” said Edsel Salvana, an infectious diseases physician at the University of the Philippines. It is uncertain whether the dengue immunisation programme actually caused any deaths – but many parents have stopped going to medical centres for vaccinations as the safety of vaccines is questioned. Nevertheless, the United Nations Children's Fund (UNICEF) stated that a child is more likely to be harmed by a VPD than by a vaccine.
In 2018, Indonesia’s influential Islamic Council issued a fatwa (religious ruling) against the measles-rubella vaccine because it contained pork gelatine. This created a vaccine hesitancy among Indonesian Muslims and derailed the country’s goal to vaccinate 70 million children. Although the council clarified the vaccine could be used if there were no available alternatives, vaccination rates in the country decreased significantly to an average of 65 percent and as low as six percent in the conservative Aceh province of Sumatra.
According to reports, for the past three years, the Philippines and Indonesia have recorded the world’s second- and third-highest rates of measles, behind India. It was reported that Indonesia’s Health Ministry is spending more than US$60 million to create campaigns aimed at convincing parents that vaccinations are mandatory. Indonesia is also currently working to create halal vaccines for its people.
In 2000, the WHO declared Malaysia to be polio-free. However, just last year, a three-month old baby in the East Malaysia state of Sabah, located on the northern portion of Borneo – was diagnosed with a vaccine-derived poliovirus (cVDPV). It is the first polio case in the country in almost three decades. The country’s Health Ministry stressed that the boy did not get polio from his vaccination, assuring parents that the cause of the cVDPV was low immunisation coverage. Parents were urged to get their children immunised to ensure “herd immunity”, which would protect the whole community.
Malaysia’s former Health Minister, Dr Dzulkefly Ahmad announced in 2019 that the government aimed to amend the law to make two of 12 scheduled vaccinations mandatory, which are for MMR (mumps, measles and rubella) and diphtheria. But with the latest change of government in Malaysia, it is unclear whether the proposed bill will be tabled in Parliament.
Many other myths regarding vaccines have been debunked by health experts such as its relation to autism and sudden infant death (SID) syndrome. Misinformation about vaccines is typically spread through social media which leads to vaccine hesitancy. There are a significant number of anti-vaccine groups on platforms like Facebook alone. The United States’ (US) Centers for Disease Control and Prevention (CDC) recommends vaccinations to protect against many infections; as without vaccines one may be vulnerable to a variety of illnesses.
Related articles:
