Since abandoning all COVID safety measures and relying on the government’s “Living with COVID-19” strategy, the United Kingdom (UK) has seen a surge in the number of people becoming infected with the virus. Although numbers are coming down now, they remain at relatively high levels.
This new wave is thought to be driven by the BA.2 sub-variant of Omicron as well as waning protection from vaccines. According to the World Health Organization (WHO), the BA.2 sub-variant of the original Omicron variant of coronavirus (now known as BA.1) has specific mutations that give it a growth advantage over BA.1.
When we have large volumes of two viruses that are genetically linked circulating in the population, there is a risk of a recombinant virus forming. This is thought to have been the case in the UK with the discovery of Omicron XE; a recombinant virus made up of the BA.1 and BA.2 sub-variants of Omicron.
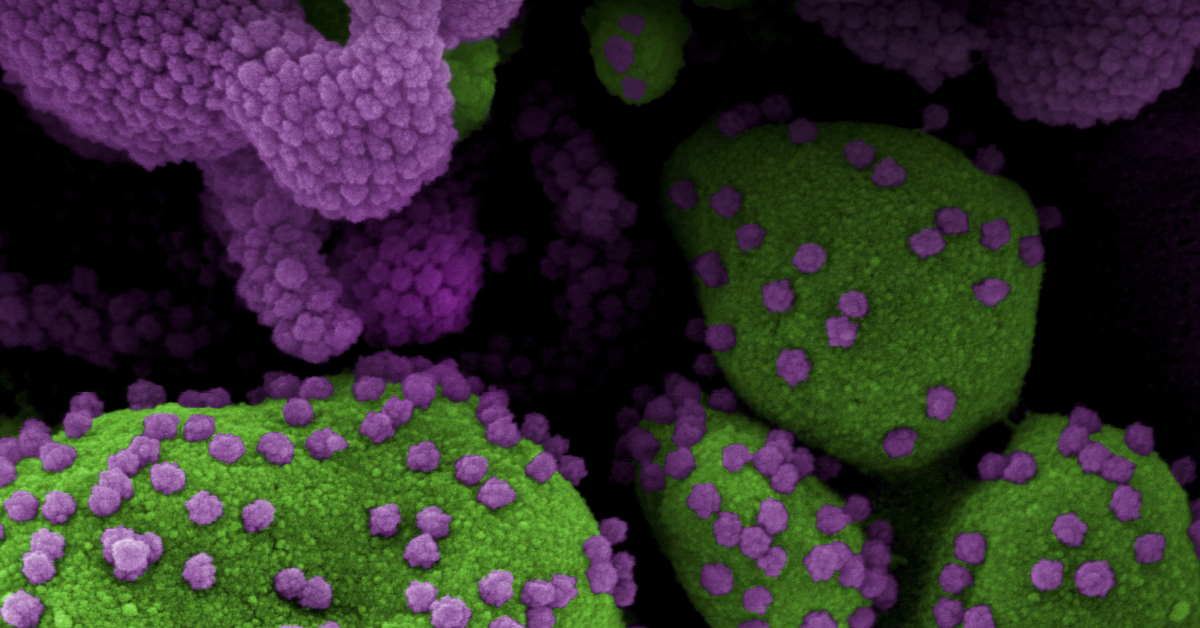
Recombinant viruses occur in instances like this when an individual is infected by two different viruses that share similar genetic material, as is the case with BA.1 and BA.2. As both sub-variants divide rapidly inside their human host cells, they can swap some of their genetic makeup and form a new “hybrid” sub-variant made up of both parent viruses. Recombination is common among coronaviruses and is expected.
Omicron XE was first detected on 19 January, 2022, and more than 600 cases have since been detected in England. And although it is too soon to say conclusively, according to the WHO, early tests suggest it has a growth advantage of approximately 10 percent when compared with BA.2.
It continues to be monitored and there is currently no reason to believe it confers any more serious illness than previous Omicron sub-variants or has any specific properties that mean it might evade the protection given by vaccines or previous infection.
For now, the WHO says it will classify Omicron XE under the Omicron family rather than as a new variant in its own right; this may change if evidence suggests that it harbours enough changes that affect disease severity, transmission or resistance to treatment.
Since its discovery, small numbers of XE have also been identified in China, India and Thailand. As the sub-variant is very new, little is known about the characteristics of the strain, but it is currently not believed to cause any new symptoms.
Omicron XE is not the only recombinant variant to have occurred. The WHO continues to monitor the XD and XF sub-variants which are both thought to be combinations of the Delta and Omicron variants of coronavirus. Only 38 cases of XF have been identified in the UK since mid-February and no cases of XD.
Just 49 cases of XD have been reported to global databases, the UK Health Security Agency said. The majority of these were found in France. Neither is thought to be any more transmissible than the original Omicron variant, and as a result, they have failed to make an impact on case numbers.
For now, the advice remains the same: ventilate indoor spaces, wear a mask when on public transport and in indoor public spaces, and get vaccinated.
Memory B Cells Persist After Third Vaccine Dose
More than two years since the pandemic began, COVID-19 still rages on with the arrival of the Omicron variant and it’s even more infectious sub-variant, BA.2. Many countries are seeing a surge in the number of people testing positive, and some of them are ending up in hospital as a result. The widely used mRNA COVID vaccines, and in particular the boosters, have been shown in numerous studies to be effective in preventing serious illness from COVID infection.
Data from the United States (US) in February 2022 showed that unvaccinated adults aged 18 to 49 were four times more likely to be hospitalised than their fully vaccinated (including having the booster) peers. Among those over 65, the unvaccinated were six times more likely to be hospitalised.
There has always been some debate about how long protection from an initial vaccine dose might last, and what effect the boosters have. Several studies have shown that the protection from infections, including symptomatic infections, offered by vaccines wanes from 90-95 percent two months after being vaccinated, to about 60 percent for Pfizer or 70 percent for Moderna, five to six months after vaccination.
There is further substantial waning after six months. It is not just protection from vaccines that lessens; we have seen people who caught COVID in the past getting infected again. If immunity wanes quickly, millions of people may be at risk for reinfection after recovery from the virus.
The immune system is complicated, and a waning immune response is generally associated with a part of it known as neutralising antibodies. Their production is triggered by either the vaccine or natural infection. They then circulate in the blood, keeping an eye out for the SARS-CoV-2 virus. If they encounter it, their job is to neutralise and destroy it before it gets a chance to enter and infect cells.
To do this, they must be able to recognise the virus. But mutations such as the ones seen in the Omicron variant mean they may not recognise their target so well, which may explain why we are seeing so many infections after people have been infected in the past or have had the vaccines – also known as breakthrough infections.
While the number of neutralising antibodies declines over time, there is another group of immune cells that studies have shown last longer, especially after booster shots – memory B cells. These cells remember the virus and recognise it should it try to infect the body again; they then signal the production of antibodies to kill both the virus and any cells it has already managed to infect.
It has always been unclear how long these might last and what effect boosters would have on them. Now, a new study has shown that the third dose of the mRNA vaccines from Pfizer or Moderna increases the power of these memory B cells that were induced by the second dose of the vaccine by not just strengthening their ability to produce antibodies, but also enabling them to produce antibodies that could help better neutralise mutated versions of the virus such as the Omicron variant.
The study states the third dose of the vaccine expands and diversifies the types of memory B cells already present from previous doses, which can respond rapidly and produce antibodies capable of clearing even diversified variants. A separate study shows the third dose of the vaccine helps stabilise the decline of antibodies and found they gave rise to longer-lasting memory B cells.