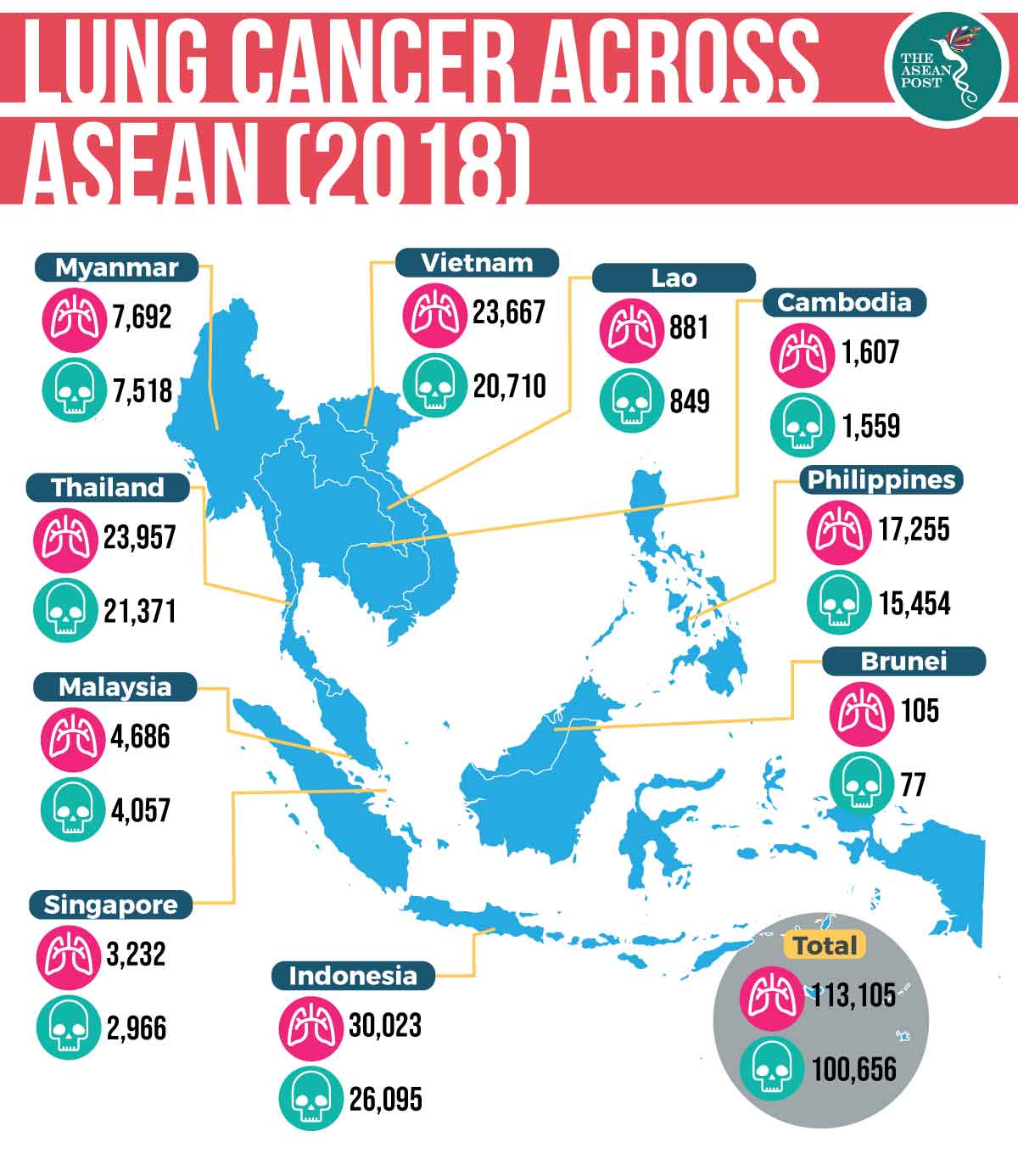
Lung cancer is the most common form of cancer with approximately 2.09 million new diagnoses every year, and is responsible for the most cancer deaths, according to the World Health Organisation (WHO). Based on data compiled by the International Agency for Research on Cancer (IARC), the disease killed nearly 1.8 million people in 2018, of which 61.4 percent of deaths occurred in the Asia Pacific region. Across ASEAN member states, the Global Cancer Observatory recorded a total of 113,105 new cases of lung cancer in 2018.
Smokers have a higher risk of getting lung cancer, which accounts for at least 80 percent of all lung cancer cases. However, environmental factors such as air pollution, occupational exposure and passive smoking also contribute to the risk.
Early detection
The Malaysian Study on Cancer Survival 2018 cites that the five-year survival rate for lung cancer across all stages is just 11 percent. According to Dr Anand Sachithanandan, consultant cardiothoracic surgeon at Subang Jaya Medical Centre in the state of Selangor in Malaysia, lung cancer is the worst performing of all cancers, with the median of survival after diagnosis a mere 6.8 months.
Unfortunately, lung cancer is asymptomatic, resulting in at least 80 percent of late stage detection. Dr Anand emphasises the need for early detection of lung cancer, “The goal of treatment for early-stage cancer is curative, where we hope to cure the patient.” Screening leads to early detection, meaning earlier treatment with greater options and increased chances of survival.
Immunotherapy
The new era of biomedical discovery is changing the way many cancers are treated. There are currently three mainstream treatments for cancer; surgical removal, radiation therapy and chemotherapy. But advanced clinical trials and studies have shown that checkpoint blockade and adoptive immunotherapy are two examples of the newest treatments.
Immunotherapy harnesses the patient’s own immune system to fight harmful intruders like cancer cells. Merck Sharp & Dohme (MSD) is leading the research of immunotherapy with over 1,000 trials, including more than 600 trials that combine the drug pembrolizumab with other cancer treatments. These trials cover over 30 tumour types including lung cancer. MSD claims pembrolizumab is a first line therapy for a subset of metastatic non-small cell lung cancers where patients can have access to the drug even before receiving chemotherapy.
Dr Kong Hwai Loong, a medical oncologist at Icon SOC Singapore at the Paragon Medical Centre said that “immunotherapy, especially pembrolizumab, has significantly and positively changed the lung cancer treatment landscape.”
In 2018, Singapore’s Health Sciences Authority approved pembrolizumab in combination with chemotherapy, as a first-line treatment for patients. According to Dr Kong, two other immunotherapy drugs, nivolumab (Opdivo) and atezolizumab (Tencentriq), are also available in Singapore for lung cancer treatment.
Pembrolizumab was also approved in Malaysia where the majority of suitable patients receive immunotherapy as their first line of treatment.
At the War on Cancer Asia Summit held in Singapore last year, MSD’s President for Asia Pacific, Dorthe Mikkelsen pointed out the importance of collaboration between all parties involved in healthcare, including governments, physicians, patients and other stakeholders “to expand patients’ access to various innovative treatments available, such as immunotherapy which benefits patients and the community as a whole.”
An investment
Cancer can also burden the healthcare system due to an ageing population and the adoption of cancer-associated lifestyle behaviours. ASEAN healthcare spending is forecasted to reach US$740 billion in 2025 and this rise would hurt the economy and healthcare standards of the region.
The cost of treatment is still a key issue around immunotherapies and the long-term cost is a major consideration for many patients. In Singapore, the cost of immunotherapy treatment ranges from SG$7,000 (US$5,200) to SG$15,000 (US$11,000) every three weeks, depending on the dosage, commented Dr Wong Seng Weng, medical director and consultant medical oncologist at The Cancer Centre in Singapore.
Since treatment is an investment, a more effective intervention will likely benefit patients and bring value to the health system. MSD turned to biomarker testing to help “predict which patients will respond to treatment, thereby managing the healthcare budget efficiently.”
With immunotherapy treatments, the overall survival rate for lung cancer patients can improve. This, in turn, benefits the healthcare system and the broader society. But physicians and healthcare providers need to help patients understand the potential benefits, harms, side effects and costs of drugs not subsidised by the government to allow patients to make an informed decision about treatment options.
Related articles:
