Is there one pandemic, or two? That was a question being asked a year ago, when wealthy countries accounting for only 15 percent of the global population had 80 percent of the COVID deaths. Could it be that the rich world was more vulnerable, somehow, because its populations were older, or more individualistic, or had forgotten to be scared of infectious disease?
Even then, some were warning that the worst was yet to come, once the disease took hold in poorer countries. World Bank analysts Philip Schellekens and Diego Sourrouille, for example, predicted a “massive shift” in disease burden to the developing world. Just in terms of demography, they said, you’d expect those countries to account for around 70 percent of deaths. As things stand, they account for a little over half of it, which is probably an underestimate due to variations in data quality – and the pandemic is far from over.
Last week saw more than 5.8 million new cases of COVID globally, the highest number yet. More than three million people have now died from COVID, according to the World Health Organization (WHO), which also reports that infections and hospitalisations in those aged 25 to 59 are increasing at an alarming rate.
“It took nine months to reach one million deaths, four months to reach two million, and three months to reach three million,” WHO director general, Tedros Adhanom Ghebreyesus, said last week.
The sharpest upticks in recent weeks have been seen in Southeast Asia – driven in large part by India – and the eastern Mediterranean and western Pacific regions, but the situation is also very bad in Latin America. People who migrated to Brazil in search of work are now reported to be fleeing the humanitarian catastrophe that is unfolding there.
Infection rates are still high in many wealthy countries – including the United States (US) and much of Europe – but the mood is more upbeat: as vaccines roll out, many people feel the worst is behind them. Some US states have rashly lifted their mask mandates. The British government gave the most optimistic signal it could think of earlier this month, when it reopened pubs.
And COVID-19 is slipping down the headlines, reflecting not just fatigue at having to respect the rules, but fatigue at the very mention of the disease. Fear concentrates the mind, but fear is dissipating; we’d rather read about Tory sleaze, or the doomed European Super League. Again, you could be forgiven for asking, is there one pandemic or two? Only now the question has an entirely different meaning. The tables have turned.
In reality, there was only ever one pandemic. We tend to think of it in terms of national impacts and responses, at best regional ones, but for it to make sense you have to stand back and look at it globally. For all its idiosyncrasies, COVID will stay true to type in at least one way: like pandemics throughout history, it will hammer the poorest hardest.
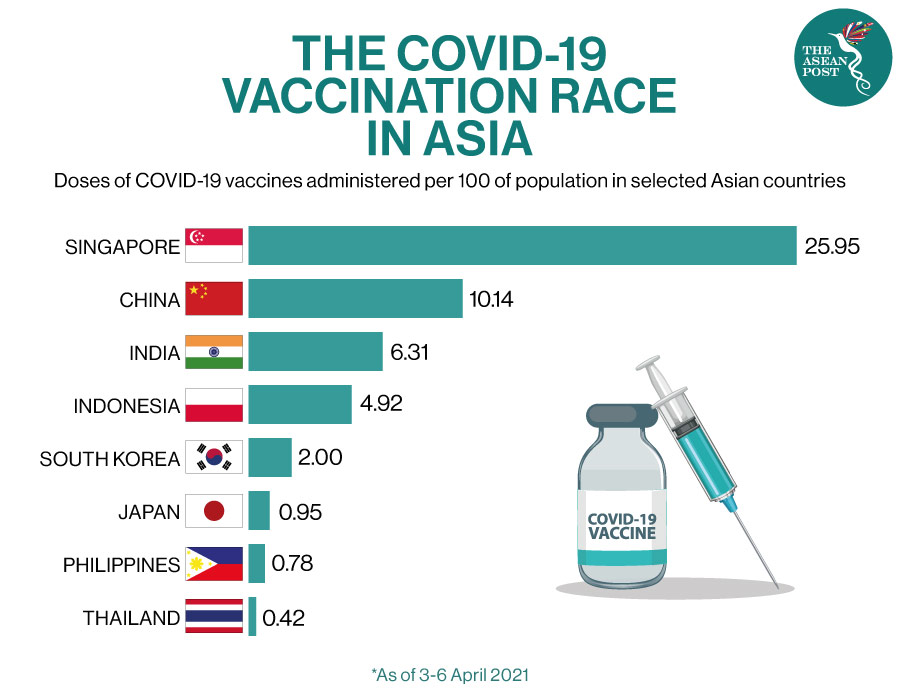
Depending on where you’re standing, there are genuine reasons to be cheerful. The vaccines are effective in mitigating the disease and there’s growing evidence that they slow its spread too. But their rollout is extremely uneven. A quarter of Americans have been fully vaccinated to date, compared with fewer than two percent of Ghanaians. An Israeli is 20 times more likely to have received a single vaccine dose than a Palestinian, and there are still countries that haven’t administered any.
There’s unevenness within countries too, in part due to vaccine hesitancy. A recent survey of US healthcare workers showed that 48 percent had yet to be vaccinated, and 18 percent didn’t intend to be. Partly because they have seen relatively few COVID deaths locally, people in Hong Kong are staying away from vaccine clinics – a manifestation of the so-called “prevention paradox”.
The recent increases in cases and deaths are partly due to the spread of new COVID variants. These are all more transmissible than the original form, first detected in China, and some of them are more lethal. There’s good reason to hope that the vaccines will continue to work against them – or can be updated to do so – but in the meantime the variants, combined with slow vaccine rollout, are pushing fragile health systems to breaking point.
Without oxygen, for example, it’s impossible to treat a severely ill COVID patient, but there’s a global shortage of the gas. In Peru, where hospitals are in crisis, Médecins Sans Frontières reports that “people in many cities queue overnight and sleep in the rough to fill up their oxygen tanks from the few working reservoirs, hoping to take care of their relatives at home”.
When a health system is paralysed, non-COVID patients are unable to get treated too, and resources are sucked away from longer-term public health campaigns – meaning that the burden of diseases such as HIV and malaria may increase. Demography is not the only reason for the developing world’s continuing vulnerability, in other words.
The COVAX facility, which was designed to offset vaccine nationalism, aims to get a first vaccine dose to at least 20 percent of the population of each participating country by the end of 2021 – though it now looks like it will fall short of that goal. Even if it hits its target, since less than a quarter of the global population is judged likely to have acquired immunity through natural infection to date, that will leave at least half of it susceptible to COVID in the short term.
The disease still mainly targets older people, and though rich countries tend to have proportionally more older people than poorer ones, in absolute terms there are far more elderly people in the developing world. India, for example, has around three times as many people aged 60 or older as Japan, though in terms of its population structure, Japan is considered the oldest country in the world. Burgeoning infection rates in the developing world therefore herald absolute, if not relative, carnage there.
We can still hope that the global death toll from COVID in 2021 will not exceed that of 2020 – as the vaccines do their work – even if it’s far from a given. But we can be confident that poorer countries will contribute most of this year’s COVID deaths. That thought alone should give us pause – and in addition we should remember that rich countries are not immune from what happens beyond their shores.
Rampant COVID in countries such as India and Brazil will shape the evolution of the virus and could cause new, even more dangerous variants to emerge, which neither our borders nor our vaccines are guaranteed to keep out. That’s why it’s too early to rest on our laurels and why vaccine equity is so important – because this is a pandemic, meaning it’s global. – The Guardian
Related Articles:
